Physician Office Compliance Manual
Making the Best Use of Office Hours; Physician Scheduling; Open Access Scheduling. Revise their policies and procedures for providing patients access to their medical records. WARNING: These manuals are templates meaning they contain sample policies and procedures. Each practice will need to adapt them to align with its specific staffing. Nov 7, 2013 - The Chief Compliance Office shall convene Compliance Committee meetings. The ACO will not pay employees, physicians, or health care. Medical Billing Compliance from AdvantEdge Healthcare Solutions. AdvantEdge offers a toll-free Compliance Hotline directly to our compliance office who will. That the Compliance Program, the Compliance Manual, employee training and.
Significant new changes to the HIPAA law require dramatic changes to each practice's Privacy and Security Compliance Manual. Those who have not updated their HIPAA manuals to comply with the HITECH requirements, which went into effect 2013, need to do so right away. It is an understatement to say that the HITECH act has changed HIPAA compliance. The biggest change to HIPAA compliance is the significant toughening of data breach notification requirements, which now not only impose larger fines and require more extensive public notifications when data is lost, but also apply to a health care provider's business associates. There are many required changes for HIPAA Compliance manuals, but here are a few of the most important ones. Pediatric practices must:.
Update all their Business Associate agreements because of the new data breach provisions and penalties. Update their Notice of Privacy Policies to address patient rights to access their medical records and be notified of data breaches. Revise their policies and procedures for providing patients access to their medical records. WARNING: These manuals are templates meaning they contain sample policies and procedures. Each practice will need to adapt them to align with its specific staffing, technology, and office operations. It is important to remember that HIPAA compliance is more than having a manual on a shelf. The policies, procedures and staff training described in the manual must be incorporated into the practice's daily operations.
The Academy's sample HIPAA Privacy and Security Compliance Manuals have been created specifically for pediatric practices and may be downloaded and adapted by AAP members at no cost. Disclaimer: This information is general in scope and educational in nature. It is not intended as legal advice. If you require legal advice, contact an attorney. The recommendations in this publication do not indicate an exclusive course of treatment or serve as a standard of medical care. Variations, taking into account individual circumstances, may be appropriate. This content is for informational purposes only.
It is not intended to constitute financial or legal advice. A financial advisor or attorney should be consulted if financial or legal advice is desired.
Upon successfully completing this chapter, you will be able to:. Spell and define the key terms. Describe what is meant by organizational structure. List seven responsibilities of the medical office manager. Explain the five staffing issues that a medical office manager will be responsible for handling.
List the types of policies and procedures that should be included in a medical office's policy and procedures manual. List five types of promotional materials that a medical office may dist. The medical office manager must be multiskilled, multitalented, and able to prioritize a variety of issues, juggle responsibilities, and communicate effectively with patients, staff, and physicians. In some settings, the medical office manager may be referred to as the business manager. Managers may be nurses, medical assistants, or administrative support personnel. Staff meeting should be scheduled at a predictable frequency and time to allow the staff to plan. Staff meetings should never be canceled except in a true emergency.
Agendas should be created prior to the meeting and posted for staff review. Staff meeting should be conducted in a private area out of patient's sight and hearing. All interruptions, except for emergencies, should be avoided.
The personnel manual should clearly state the attendance policy for staff meetings. In addition, some offices include attendance as a duty in each employee's job description. To improve attendance at staff meetings, consider serving food or including an educational presentation. Involve staff as much as possible when setting the meeting agenda. Title VII of the Civil Rights Act prohibits discrimination in the workplace.
To ensure that hiring practices are fair and nondiscriminatory, be careful and consistent in the types of questions asked in an interview. You You may ask work related questions like, 'Are you proficient in typing?' Avoid questions that might give the appearance of discrimination. You may not ask applicants their age, race, religion, or marital status.
You cannot ask about children, daycare, or plans for future children. Only after creating or reviewing an existing job description can you begin the process of interviewing and hiring a new employee. All applicants should complete an application. State laws vary regarding the types of questions that can be asked on applications. If your medical facility requires a criminal background check and drug testing, the form should include this information with a place for the applicant to give necessary permission with a signature. Any employee application form should be reviewed by legal counsel prior to its use. Before interviewing an applicant, prepare a list of questions.
Under law, you are not permitted to ask about certain topics. During the interview, assess the applicants ability to do the following:.
Perform technical skills. Treat patients in a caring manner. Communicate in a professional yet friendly manner. Remain flexible Be consistent and fair when selecting the best candidate.
Having to terminate, or fire, an employee is never an easy or pleasant task. It is essential that policies regarding termination be followed precisely. All disciplinary actions must be clearly and objectively stated.
Terminating employees for unlawful reasons or failing to follow the organization's termination policy can result in lawsuits against you and the practice. Some reasons for termination include:. Excessive tardiness or absenteeism. Inappropriate dress or behavior. Endangering patients.
Lying or stealing. Falsifying medical records or time sheets. Breaching patient confidentiality. Every business needs written rules and regulations to ensure its practices are within legal and ethical boundaries.
Employees need written procedures to ensure consistency in the practices of the business. It is the office manager's responsibility to coordinate the orientation and training of any new employee. Most organizations create a policy and procedures manual that is written, maintained, and regarded as one document.
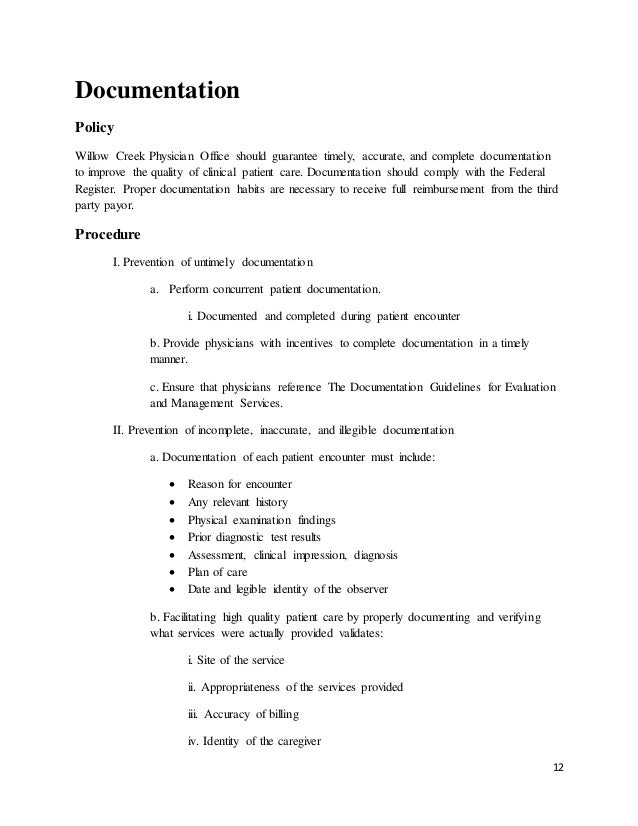
A policy is a statement regarding the organization's rules on a given topic. A procedure is a series of steps required to perform a given task. Policies and procedures must be written in a clear, concise, and understandable format. The medical office manager is often responsible for developing and distributing promotional literature for the practice. Examples of promotional materials are:.
Physician Office Compliance Manual
Education pamphlets and booklets for patients. Be sure to use educational information that has been accredited or approved by an appropriate authority. Practice brochures. Newsletters. Holiday cards. Birthday cards.
Newspaper articles. Yellow pages. Direct mail. Business cards Follow these guidelines when creating promotional material:. Double-check all spelling and grammar. Ensure accuracy. Use clear and specific language.
Avoid abbreviations and complex medical terms. Use brightly colored materials. If you are using a commercial printer, be sure to review the proofs carefully before the final printing. A budget is a financial planning tool that helps an organization estimate its anticipated expenditures and revenues. Budgeting has many purposes for an organization:. Forcing the manager and physician to plan.
Causing managers and staff to become cost conscious. Promoting communication among staff and managers. Helping the organization achieve a financial goal. The medical office generally has both an operating and a capital budget.
Compliance Plan For Physician Office
Operating budgets consist of all cost to run the office. Capital budget consists of the large outlays of money. The medical office manager must keep this staff up-to-date on medical procedures, drugs and vaccines, insurance coding and billing regulations, and any other topics that promote good patient care. In addition to the topics, annual education is usually conducted on cardiopulmonary resuscitation (CPR), infection control, and fire in electrical safety.
Most allied health professionals are required to accumulate continuing education units (CEUs). As the medical office manager, you should select an educational topic for each month. In some offices, the educational topic is covered during the monthly staff meetings, whereas other offices have separate educational programs. In addition to formal education programs, there are other ways to keep your staff up-to-date.
For instance, educational videos and DVDs can be rented or purchased for staff viewing; consider developing a post test to assess for comprehension. Also, many professional magazines have continuing education articles many professional magazines have continuing education articles on various topics, usually accompanied by a post test. Finally, staff members should be sent to one or two seminars a year. Outside seminars help increase employee productivity, self-esteem, and retention.
Doctors today face challenges that those of a generation ago never imagined. Physicians are at risk for malpractice suits and must use sound practices to decrease this risk. Physicians need malpractice insurance to protect them from financial loss in the event of a successful lawsuit or settlement. Nurses also carry malpractice insurance, and many allied health professionals are now opting for coverage. As office manager, you should assess the coverage needs of your employees and investigate the possibility of a policy that would cover any employees who need it. Insurance is a large expense but one that a medical practice must incur.
Even in the safest settings, undesirable things can happened to patients. These events sometimes result from human error, or they may be idiopathic. Idiopathic means that something occurred for unknown reasons and was unavoidable. Incident report must be completed even if no injury resulted from an event. A few examples of situations requiring an incident report are:. All medication errors.
All patient, visitor, and employee falls. Drawing blood from a wrong patient. Mislabeling of blood tubes or specimen. Incorrect surgical instruments counts following surgery. Employee needlesticks. Workers' compensation injuries The rule of thumb is, when in doubt, always complete it incident report.
Although every agency has its own form, the following data are always included in an incident report:. Name, address, and phone number of the injured party. Date of birth and sex of the injured party.
Date, time, and location of the incident. Brief description of the incident and what was done to correct it. Any diagnostic procedures or treatments that were needed. Patient examination findings. Names and addresses of witnesses. Signature and title of person completing the form. Physician's and or supervisor's signature as per policy.
When completing an incident report, follow these guidelines: 1. State only the facts.
Do not draw conclusions or summarize the event. Write legibly and sign your name legibly. Be sure to include your title.
Complete the form in a timely fashion. In general, incident reports should be completed within 24 hours of the event. Do not leave blank spaces on the form.
If a particular section of the report does not apply, write not applicable. Never photocopy and incident report for your own personal record. Never place the incident report in the patient's chart. Never document in the patients chart that an incident report was completed.
Only document the event in the patients chart. By writing in the medical record that an incident report was completed, that opens the potential for lawyers to subpoena the incident report, should there be a lawsuit. After incident reports are completed, they are reviewed and tracked to highlight specific patterns. The resulting statistical data can be used to identify problem areas, which can be corrected through quality improvement programs. Examples of statistical data that can be found in incident reports include:. Particular days of the week when most negative events happened.
Most common area for patient falls. Medications that are routinely given incorrectly. The age group most likely to have problems. Incident reports should be kept in a special file in the manager's office. One of the most challenging problems for risk managers is to prevent noncompliance with regulatory agencies.
Numerous agencies regulate health care settings, and these rules and regulations change frequently. You can stay up-to-date with new changes by reading newsletters from these organizations, attending the state and local professional meetings, and frequently visiting various professional websites. Every state has a website that will link you to legislative action. Read these regularly. Each office should have legal counsel who can assist in interpreting legal issues.
The Joint Commission is a private agency that sets health care standards and evaluates an organization's implementation of those standards for health care settings. The Joint Commission surveys these centers and then assigns them an accreditation title. A survey is an on-site evaluation of the organization's facility and policies. Participation in The Joint Commission is voluntary for health care organizations; without accreditation, however, the health care organization may not be eligible to participate in particular federal and state funded programs, such as Medicare and Medicaid. The size and complexity of an organization's quality improvement program depends on the organization's particular needs. A few examples of quality issues that can be monitored in the physician offices are:. Patient waiting times.
Unplanned returned patient visits for the same ailment or illness. Misdiagnosed illnesses that are detected by another partner in the practice. Patient or family complaints. Timely follow-up telephone calls to patients.
Patient falls in physician's office or office building. Mislabeled specimens sent to the laboratory. Blood specimens that are coagulated or contaminated. All organizations can improve their delivery of patient care. Suggestions for improving care can come from many resources, including the following:.
Office managers. Physicians. Other employees. Patients. Incident report trending The person responsible for quality improvement in the medical office reviews all quality improvement problems or potential problems and selects the one to be addressed first.
Problems given top priority are those that are high (risk most likely to occur) and those that are most likely to cause injury to patients, family members, or employees. After implementation, the solution must be evaluated to determine whether it worked and, if so, how well. Quality improvement monitoring plans have three elements:.
Source of monitoring, that is, where the numerical data will be obtained. Frequency of monitoring, that is, how often the data will be monitored and tallied. Person responsible for monitoring, that is, who collects the data and presents the results in graphic form, allowing for easy comparison of data from before and after implementation of the solution.